Sickle Cell Disease: A Guide for Junior Doctors
- Taimoor Khan
- Oct 16, 2024
- 5 min read
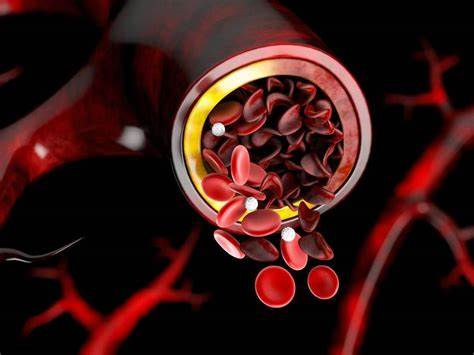
Sickle Cell Disease (SCD) is a group of inherited hemoglobinopathies that primarily affects individuals of African, Mediterranean, or Middle Eastern descent. Patients with SCD are prone to complications like vaso-occlusive crises, acute chest syndrome, and infections. For junior doctors in emergency medicine, managing these complications quickly and effectively is crucial. This post will guide you through the key aspects of history-taking, examination findings, investigations, and management plans for SCD, drawing from reliable sources.
History Taking: Key Questions to Ask
· Presenting Complaint
· Pain episodes (Vaso-occlusive crisis): Ask about the nature, onset, and severity of the pain. Sickle cell crises often cause severe, sharp, or throbbing pain, commonly in the bones (e.g., arms, legs, chest). Explore:
o How long has the pain lasted?
o Where is it located? Is it in more than one site?
o Have they experienced similar episodes before?
· Infection history: Sickle cell patients are prone to infections, especially those caused by encapsulated organisms (e.g., Streptococcus pneumoniae), due to splenic dysfunction. Ask about fever, cough, or any recent infections.
· Breathing difficulties (Acute Chest Syndrome): Ask about chest pain, difficulty breathing, and any recent respiratory infections. Acute chest syndrome is a life-threatening emergency in SCD.
· Neurological symptoms: Ask about any recent neurological deficits like weakness, numbness, or difficulty speaking, as SCD patients are at risk of stroke.
· Previous crises and treatments: How often do they experience pain crises? Have they been hospitalized previously? What medications or treatments helped them in the past?
· Past Medical History
· Previous sickle cell complications: Have they had episodes of acute chest syndrome, stroke, or priapism? Knowing their past medical history will help assess the severity of the current episode.
· Splenectomy status: Have they had a splenectomy or are they functionally asplenic? This influences susceptibility to infections.
· Medication use: Are they on hydroxyurea or any other disease-modifying treatment? Hydroxyurea reduces the frequency of painful episodes.
· Vaccination history: Ask if they are up-to-date with vaccinations, particularly against encapsulated bacteria (e.g., Haemophilus influenzae, Neisseria meningitidis, Streptococcus pneumoniae).
Family and Social History
· Family history of SCD or similar hemoglobinopathies: This can provide insight into the genetic background and risk factors.
· Social factors: Assess for stressors, dehydration, or exposure to cold weather, as these can trigger vaso-occlusive crises.
Examination Findings
· General Appearance
· Pallor and jaundice: Look for signs of anemia and hemolysis. Jaundice may indicate ongoing hemolysis due to the breakdown of sickled red cells.
· Painful areas: Inspect and palpate areas of reported pain. These may involve the bones, joints, or muscles, especially in long bones and the spine.
· Vital signs: Check for tachycardia, hypotension (signs of shock), tachypnea, or fever, which may indicate infection or acute chest syndrome.
· Cardiovascular and Respiratory Examination
· Tachypnea and hypoxia: In patients with chest pain or shortness of breath, monitor oxygen saturation. Hypoxia or abnormal breath sounds may suggest acute chest syndrome.
· Cardiac findings: Patients with chronic anemia may have flow murmurs due to increased cardiac output. Be vigilant for signs of heart failure, particularly in older patients.
· Abdominal Examination
· Splenomegaly or splenic sequestration: Palpate for an enlarged spleen, especially in younger patients. Splenic sequestration can cause severe anemia and shock.
· Liver and gallbladder: Hepatomegaly and tenderness may indicate hepatic sequestration or cholelithiasis (common in SCD due to chronic hemolysis).
· Neurological Examination
· Stroke signs: Perform a quick neurological examination if the patient presents with any altered mental status, focal neurological deficits, or seizures, as these may be early signs of stroke.
· Extremities
· Joint swelling and tenderness: Painful joints and limbs are common in vaso-occlusive crises. Check for warmth, redness, and swelling, which may suggest secondary infection or infarction.
Investigations: Ensuring Proper Diagnosis and Treatment
Baseline Investigations
· Full blood count (FBC): Check for anemia (low hemoglobin) and leukocytosis, which may suggest infection or inflammation. The baseline Hb for SCD patients is typically lower than the general population, but a sudden drop may indicate splenic sequestration or acute hemolysis.
· Reticulocyte count: Elevated reticulocyte counts suggest increased red blood cell production in response to hemolysis or anemia.
· Blood film: A peripheral blood smear can show characteristic sickle-shaped cells and Howell-Jolly bodies (suggestive of splenic dysfunction).
· Additional Blood Tests
· Lactate dehydrogenase (LDH): Elevated LDH levels are markers of hemolysis.
· Bilirubin: Total and direct bilirubin levels help assess the degree of hemolysis and hepatic involvement.
· C-reactive protein (CRP) and blood cultures: Consider these in febrile patients to rule out infections.
· Renal function (U&Es): Assess kidney function as SCD can lead to renal complications, especially in patients with dehydration or crisis.
· Imaging
· Chest X-ray: Obtain a chest X-ray in patients with respiratory symptoms to rule out acute chest syndrome, pneumonia, or pulmonary infarction.
· Ultrasound (Abdomen): May be indicated if you suspect splenic sequestration or cholelithiasis.
· CT or MRI (Head): Consider imaging for patients with neurological symptoms suggestive of stroke.
Management Plan: Acute Care in the Emergency Setting
Initial Stabilization
· Oxygen therapy: Administer supplemental oxygen if the patient is hypoxic or shows signs of respiratory distress.
· IV fluids: Start intravenous fluids to correct dehydration, which can exacerbate a vaso-occlusive crisis. Use caution not to overload fluids, especially in patients with acute chest syndrome.
· Analgesia: Pain control is critical. Administer opioid analgesics (e.g., morphine, fentanyl) promptly. Avoid NSAIDs in patients with renal impairment.
· Specific Management
· Vaso-occlusive crisis:
o Provide aggressive hydration and analgesia.
o Consider blood transfusion if there is evidence of severe anemia or acute organ damage (e.g., stroke, acute chest syndrome).
· Acute chest syndrome:
o This is a medical emergency requiring immediate intervention.
o Treat with oxygen, broad-spectrum antibiotics (to cover Streptococcus pneumoniae and Mycoplasma pneumoniae), and consider exchange transfusion if the patient is deteriorating.
· Stroke:
o Immediate exchange transfusion is indicated to reduce the percentage of sickled cells.
o Consult neurology and hematology for ongoing management.
· Infections:
o Administer broad-spectrum antibiotics if infection is suspected.
o Empiric coverage should include ceftriaxone or cefotaxime, and consider adding macrolides for atypical organisms if there’s respiratory involvement.
Long-term Management and Prevention
Hydroxyurea: Patients on hydroxyurea should be encouraged to continue their medication. Hydroxyurea increases fetal hemoglobin (HbF) levels, reducing the frequency of sickling episodes.
Blood transfusions: Consider chronic transfusion therapy for patients with recurrent complications, especially strokes or acute chest syndrome.
Vaccinations: Ensure the patient is up-to-date with vaccines, including Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae.
Sickle Cell Disease is a complex condition that requires prompt, targeted interventions in the emergency department. By asking the right history-taking questions, performing a thorough examination, and selecting appropriate investigations, junior doctors can manage both the acute and chronic complications of SCD. Early recognition and intervention, especially in cases of acute chest syndrome and stroke, can significantly improve outcomes.
Comments